**Marissa has been a huge supporter of MOVE for many years now, we are so excited to announce she will also be joining the Neuromotion Physiotherapy team as a registered massage therapist. If you have any questions about massage therapy or would like to book a session, contact them at victoria@neuromotionphysio.com!
Written by Marissa Hoen | February 17 2021
As a practicing registered massage therapist (RMT), I have seen people with a wide variety of conditions find relief through massage. There are those who come in for a tune up- to relax and discover where they hold tension, and there are also those with pain- seeking help to find the cause or relief of an already diagnosed condition. In this post I hope to clarify when you would go to see an RMT, and what we can actually do for you!
Massage helps your body heal itself
I like to compare a massage treatment to exercise: just one workout probably isn’t going to change your life (though it’s entirely possible!). While one workout can make us feel empowered, motivated, and give us a lovely endorphin rush, it is when we become consistent in our physical activity that we really start reaping the benefits. This is also true when using massage as a treatment for a specific condition. Only when treated consistently and effectively can one find long-term relief through massage*. In my experience, the greatest impact that I’ve seen in my clients is when they apply what they’ve learned in treatment to their day to day- whether that be changing their desk set-up, breathing with the diaphragm, or doing those lunges!
*Certain conditions, such as headaches caused by muscular tension, can be greatly improved by just one treatment, however if the predisposing factors are not addressed the condition is likely to return.
What are some of the benefits of massage?
Decrease stress- on a physiological level. Even just 7 minutes of hand massage was shown to decrease cortisol and promote feelings of relaxation and safeness (Maratos, 2017).
Decrease pain and improve function. Studies show improvements in musculoskeletal pain (specifically low back, shoulder, and knee arthritis) and function following massage therapy treatments, though in most cases the effects are not long lasting (Bervoets et al., 2015). Combining exercise and massage has been shown to be more effective than massage alone for low back pain (Joseph et al., 2018). Neurological pain and function related to MS, Parkinson’s, or Stroke can also be improved through gentle massage (Backus et al., 2016; Angelopoulou et al., 2020).
Increase blood flow- Depth of massage will affect the amount of blood to different tissue types. Certain conditions, such as chronic tendinopathies, benefit from increased blood flow to speed the healing process.
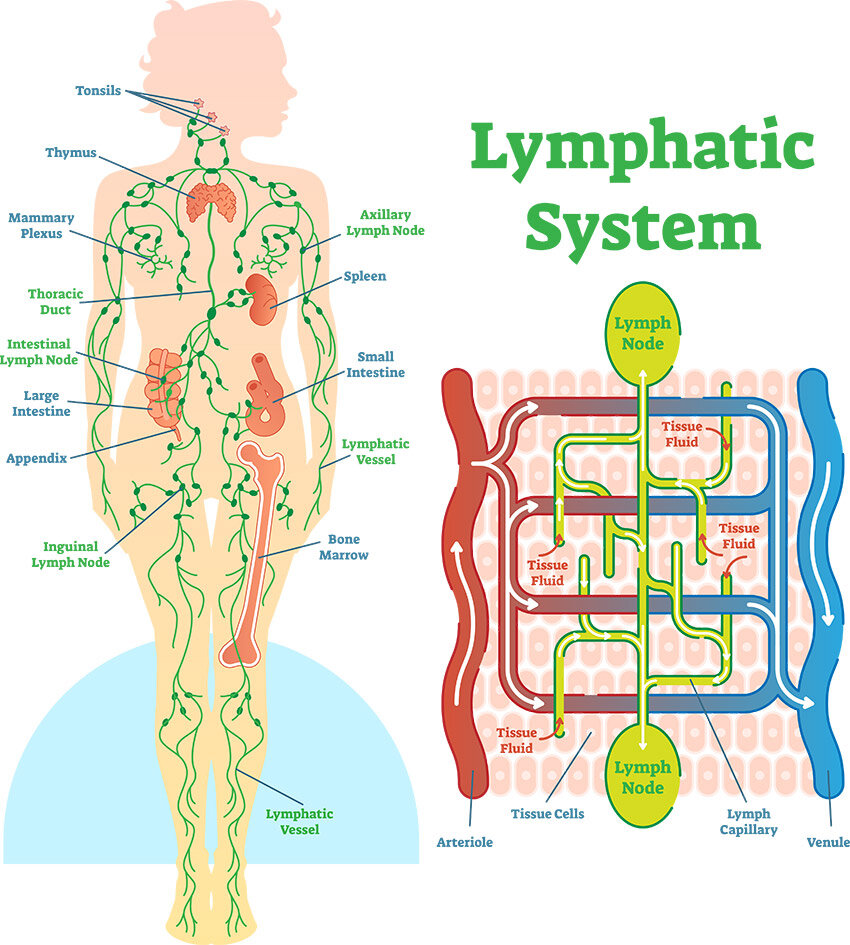
Reduce swelling- Joint swelling can be reduced through methods targeted to improve lymphatic flow (Goats 1994). Manual lymph drainage is used by many practitioners, though some are more highly trained in this method than others!
Reduces muscle bulk loss in those with nerve injuries (Goats 1994)- this ties back into the increase in blood flow. If your muscles don’t respond to your internal signals, external stimulation in the form of massage can help to keep muscles healthy.
Decrease spasticity. Massage has been shown to decrease spasticity in people who have had a stroke (Thanakiatpinyo et al., 2014), those with spastic cerebral palsy (Mahmood et al., 2019; Hernandex-Reif et al., 2005). The effect of massage on MS-related spasticity is not yet clear, as some studies report no changes in spasticity after treatment- despite the improvements in fatigue and pain (Backus et al., 2016).
If I have chronic pain, why see an RMT?
Certain clients with chronic pain find that after a treatment they have more mobility and energy to try movements I’ve suggested. Beyond this, my clients find that they are more thoughtful about their movement habits and if they know that they have another appointment soon, they are more likely to move their bodies in ways that support their condition. As RMTs, we have a great amount of one-on-one time to ensure you receive the treatment you need as well as address certain areas of daily life that may be worsening symptoms. Pain is complex, and is influenced by emotional states, physical activity, repetitive strains, thought patterns, and more. As an RMT, my goal is to listen, apply my knowledge, and provide my clients with support- so they know they are not alone. We are a team with a common goal: to get you feeling better, moving more (or less if you’re overdoing it!), and to allow your body to heal. Though massage can’t cure these chronic conditions, in our treatments you will learn ways to understand and work with your body.
In summary, what you take out of the treatment room is just as important as what happens in it. I hope each of my clients leaves the treatment with:
Stress reduction techniques
Movements specific to them
Feelings of support
Enjoyment of a time dedicated to relaxation, a time that is just for them!
Resources:
If the financial aspect of massage therapy is holding you back from booking an appointment, the West Coast College of Massage Therapy has a student clinic with 45 minute treatments for $40. By going to this college, you are both helping a student become a better future practitioner and receiving a safe and relaxing treatment. They also offer a discount to seniors over 65 and active military members. As this is a student clinic, supervisors (RMTs) may come into the treatment room to observe and give advice to the students. Here is a link to their website: https://collegeofmassage.com/victoria/clinic/book-appointment/
If this price is still a barrier, self-massage or massage by a friend is a great starting point. Check out youtube for some basic neck and shoulders massage, or join my yoga class on saturday mornings where we do lots of self-care and massage. You don’t need to be treated by a trained professional to feel the emotional benefits of a massage. (For more specific conditions and to ensure safety however, I would highly recommend booking with an RMT.)
References
Angelopoulou, E., Anagnostouli, M., Chrousos, G. P., & Bougea, A. (2020). Massage therapy as a complementary treatment for Parkinson’s disease: A systematic literature review. Complementary Therapies in Medicine, 49, 102340-102340. https://doi.org/10.1016/j.ctim.2020.102340
Bervoets, D. C., Luijsterburg, P. A., Alessie, J. J., Buijs, M. J., & Verhagen, A. P. (2015). Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: A systematic review. Journal of Physiotherapy, 61(3), 106-116. https://doi.org/10.1016/j.jphys.2015.05.018
Goats G. C. (1994). Massage--the scientific basis of an ancient art: Part 2. Physiological and therapeutic effects. British journal of sports medicine, 28(3), 153–156. https://doi.org/10.1136/bjsm.28.3.153
Schroeder, B., Doig, J., & Premkumar, K. (2014). The effects of massage therapy on multiple sclerosis patients’ quality of life and leg function. Evidence-Based Complementary and Alternative Medicine, 640916-8. https://doi.org/10.1155/2014/640916
Sefton, J. M., Yarar, C., Carpenter, D. M., & Berry, J. W. (2011). Physiological and clinical changes after therapeutic massage of the neck and shoulders. Manual Therapy, 16(5), 487-494. https://doi.org/10.1016/j.math.2011.04.002
Mahmood, Q., Habibullah, S., & Babur, M. N. (2019). Potential effects of traditional massage on spasticity and gross motor function in children with spastic cerebral palsy: A randomized controlled trial. Pakistan Journal of Medical Sciences, 35(5), 1210-1215. https://doi.org/10.12669/pjms.35.5.478
Maratos, F. A., Duarte, J., Barnes, C., McEwan, K., Sheffield, D., & Gilbert, P. (2017). The physiological and emotional effects of touch: Assessing a hand-massage intervention with high self-critics. Psychiatry Research, 250, 221-227. https://doi.org/10.1016/j.psychres.2017.01.066
Hernandez-Reif, M., Field, T., Largie, S., Diego, M., Manigat, N., Seoanes, J., & Bornstein, J. (2005). Cerebral palsy symptoms in children decreased following massage therapy. Early Child Development and Care, 175(5), 445-456. https://doi.org/10.1080/0300443042000230546
Joseph, L. H., Hancharoenkul, B., Sitilertpisan, P., Pirunsan, U., & Paungmali, A. (2018). Effects of massage as a combination therapy with lumbopelvic stability exercises as compared to standard massage therapy in low back pain: A randomized cross-over study. International Journal of Therapeutic Massage & Bodywork, 11(4), 16-22. https://doi.org/10.3822/ijtmb.v11i4.413
Thanakiatpinyo, T., Suwannatrai, S., Suwannatrai, U., Khumkaew, P., Wiwattamongkol, D., Vannabhum, M., Pianmanakit, S., & Kuptniratsaikul, V. (2014). The efficacy of traditional thai massage in decreasing spasticity in elderly stroke patients. Clinical Interventions in Aging, 9, 1311-1319. https://doi.org/10.2147/CIA.S66416